The experience of pain, with its sharpness and persistence, has shadowed the human journey since the dawn of time. Over millennia, as cultures evolved, societies transformed, and medical science progressed, humanity’s battle with pain has been marked by periods of monumental shifts and subtle transitions.
From herbs to opiates, from acupuncture to deep brain stimulation, the ways to manage and suppress pain have been diverse. In recent years, the emergence of naltrexone, particularly in its low-dose form, has been a noteworthy chapter in this continuing narrative. Its promising results have raised an inevitable query: Just how swiftly can naltrexone alleviate pain?
Naltrexone’s Essence
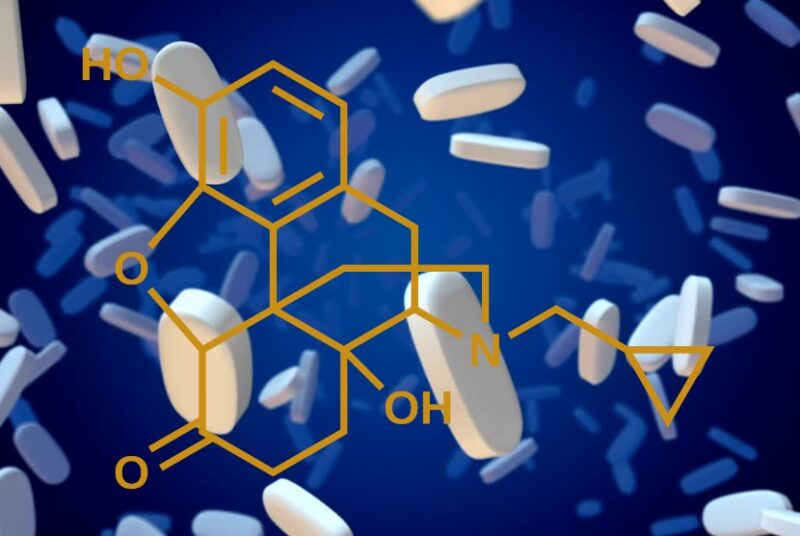
At its foundation, naltrexone stands as a staunch adversary to opioids. Both naltrexone and naloxone are classified as an opioid antagonist, its primary role is to latch onto opioid receptors in the body. But unlike its opioid counterparts, it doesn’t induce the sensations of euphoria or pain relief.
In the early days, its mainstay use was as a barrier against the intoxicating and addictive impacts of opioids and alcohol. However, the narrative takes a twist. While blocking the effects of pain relief might sound like the antithesis to pain management, a closer inspection reveals a broader picture brimming with potential.
Low-Dose: A Paradigm Shift
In the realm of pain management, naltrexone’s traditional dosage takes a backseat. Instead, the spotlight shines on Low-Dose Naltrexone or LDN. Administered in minute quantities—significantly less than dosages employed against addiction—it exhibits an altered behavioral profile. The underlying mechanisms of LDN, though not entirely delineated, hint at novel therapeutic pathways.
Over the years, extensive studies have evaluated LDN’s potential in managing an array of health conditions, spanning from autoimmune disorders to relentless chronic pain. Preliminary findings emphasize LDN’s capacity to recalibrate the immune system and diminish inflammation. Such capabilities signal potential breakthroughs in alleviating pain.
Deciphering the Timeline of Relief
The pivotal question at hand revolves around naltrexone’s speed of action. Several facets influence this:
- Dosage Dynamics: LDN, typically prescribed in daily doses ranging between 1.5mg and 4.5mg, has a responsiveness that might oscillate based on the dosage magnitude.
- The Specific Affliction: LDN exhibits potential in managing diverse conditions, such as fibromyalgia, multiple sclerosis, or Crohn’s disease. Consequently, its effectiveness and onset time may vary with the underlying ailment.
- The Individual Blueprint: Each human is a unique assembly of biology and experiences. Consequently, the timeline for LDN’s impact can range vastly among individuals.
While clinical data suggests a noticeable improvement within weeks of commencing LDN, individual accounts are varied. Some report discernible relief in days, while others may wait months before experiencing any change.
LDN’s Underlying Mechanisms
To fathom how swiftly naltrexone acts, it’s pivotal to navigate its modus operandi:
- Elevation of Endorphins: Fondly termed the body’s innate pain-relieving agents, endorphins experience a surge with LDN, potentially enhancing pain mitigation.
- Dousing Inflammation: Chronic pain often dances with inflammation. LDN, by influencing specific immune pathways, might curtail inflammatory processes.
- Modulating Opioid Receptors: By momentarily obstructing opioid receptors, LDN could amplify receptor sensitivity, thus augmenting the body’s inherent pain management.
From Clinical Trials to Personal Journeys: The Human Experience with LDN

While the rigors of scientific research provide a structured and systematic approach to understanding the effects of Low-Dose Naltrexone (LDN), the mosaic of individual stories completes the picture. These personal narratives, brimming with authenticity and lived experiences, offer perspectives that transcend data points and statistical analyses. For many, embarking on the LDN journey isn’t solely about seeking refuge from persistent pain.
Their testimonials often echo enhanced vigor, an uplifted mood, and a rejuvenated sense of purpose. In a realm often dominated by numeric pain scales, these accounts spotlight the holistic, multi-dimensional benefits of LDN — from reviving one’s zeal for life to fostering emotional resilience. In essence, these personal journeys underscore the transformative potential of naltrexone, not just as a pain moderator, but as a catalyst for comprehensive well-being.
Treading with Caution: The Imperative of Informed Decision-making
Every medicinal intervention, irrespective of its potential, comes with its share of considerations. LDN, despite its promising attributes, is no exception. Those venturing its path might occasionally encounter sleep disturbances, ranging from difficulty in falling asleep to abrupt wakefulness. Vivid dreams, an unusual yet reported side-effect, can either be fascinating or jarring, based on one’s perception.
Other potential hiccups include headaches — ranging from mild to severe — and episodes of nausea that might disrupt daily activities. Given this backdrop, the importance of medical counsel cannot be overstated. An informed decision, rooted in a thorough understanding of potential risks, benefits, and individual health dynamics, remains paramount. It’s not just about commencing LDN; it’s about ensuring its alignment with one’s broader health landscape, other medications, and overall wellness goals.
FAQs
Can LDN be taken alongside other pain medications or therapies?
Yes, in many cases, LDN can be taken alongside other pain medications or therapies. However, it’s essential to consult with a healthcare professional to ensure there are no adverse interactions or side effects. It’s especially crucial if you’re on opioid painkillers since LDN is an opioid antagonist.
How is Low-Dose Naltrexone administered?
LDN is typically administered orally in the form of a pill. Some patients may be prescribed a compounded liquid form, depending on their needs and the recommendation of their healthcare provider.
Are there any dietary restrictions or considerations when taking LDN?
There are no specific dietary restrictions associated with LDN. However, it’s always a good idea to discuss any dietary supplements, herbal treatments, or specific diets you’re following with your healthcare provider to ensure there aren’t any unforeseen interactions or considerations.
Can pregnant or breastfeeding individuals use LDN for pain management?
The safety of LDN during pregnancy and breastfeeding hasn’t been extensively studied. It’s essential to consult with a healthcare professional if you are pregnant, planning to become pregnant, or breastfeeding before starting or continuing LDN.
Are there any long-term studies on the effects of using LDN?
While there have been numerous studies on the short-term effects and benefits of LDN, long-term studies are still ongoing. As with any medication, the long-term effects can vary among individuals, so regular check-ups with a healthcare provider are essential.
Is LDN covered by health insurance?
Coverage for LDN varies by insurance provider and plan. Some insurance plans might cover it if prescribed for FDA-approved uses, like addiction treatment, but may not cover it for off-label use, such as pain management. It’s crucial to check with your insurance company regarding coverage and any out-of-pocket costs.
Conclusion
Pain management, with its layered complexities and nuances, has long been a subject of exploration, innovation, and evolution. As the chronicles of pain relief and human endurance unravel, LDN stands out as a contemporary protagonist — offering solace to many who’ve meandered through the maze of conventional treatments without respite. However, while its efficacy might oscillate across individuals, its potential in redefining pain management trajectories is palpable.
Its promise isn’t just tethered to its rapidity of action, but to its broader, transformative impact on an individual’s life quality. But, as we marvel at its potential, a pivotal reminder emerges: The essence of effective pain management isn’t just about the right medication or treatment. At its heart, it’s about individualized care, a collaborative patient-practitioner relationship, and an overarching commitment to holistic well-being.
