In the world of pharmacology, understanding the unique characteristics of different medications is vital. Naltrexone and Naloxone may sound similar, and indeed, they are both critical in addressing opioid addiction.
However, the differences between these two drugs are far more than just the letters that make up their names. In this blog post, we’ll explore these differences in detail, delving into the mechanisms of action, uses, side effects, and clinical implications of each drug.
Overview of Opioid Antagonists
Before diving into the specifics of Naltrexone and Naloxone, it’s essential to understand the broader category they both belong to – opioid antagonists. In general, opioid antagonists are a class of drugs that counteract the effects of opioid drugs on the body.
What are Opioid Antagonists?
Opioid antagonists block the effects of opioids in the body, including drugs like heroin and prescription painkillers like oxycodone. They work by binding to the same receptors in the brain that opioids bind to, but instead of stimulating the receptor (which is what opioids do), they block it. This action prevents opioids from exerting their effects and can even reverse the effects of opioids already in the system.
- They do not produce a “high” or cause addiction.
- They are often used in emergency situations to reverse an opioid overdose.
- They are also used as a part of long-term treatment strategies for opioid addiction.
The important thing to note is that while both Naltrexone and Naloxone are opioid antagonists, they are used in different ways and have unique characteristics that make them suitable for different situations.
The Mechanism of Action
The mechanism of action of opioid antagonists involves the opioid receptors in the brain and nervous system. When opioids bind to these receptors, they trigger a release of dopamine, which creates a sense of euphoria or a “high.” This euphoria is what makes opioids highly addictive.
Opioid antagonists work by binding to these same receptors but without triggering a dopamine release. This prevents opioids from binding to the receptors and negates their effects. It’s this mechanism of action that is fundamental to the roles of Naltrexone and Naloxone in managing opioid addiction and overdose.
Naltrexone: The Long-term Solution
Naltrexone is primarily used as a long-term treatment option for individuals struggling with opioid and alcohol addiction. It is not useful in treating an acute opioid overdose but rather helps in maintaining abstinence after detoxification.
Naltrexone and its Role in Addiction Treatment
Naltrexone is a once-daily medication, often administered as a pill or monthly injection, used to help people maintain abstinence from opioids or alcohol. By blocking the euphoric and sedative effects of these substances, Naltrexone can reduce the cravings and prevent relapse.
- It’s used as part of a comprehensive treatment plan that often includes counseling and participation in social support programs.
- For individuals with opioid addiction, it’s usually administered after detoxification has been completed.
- For those with alcohol addiction, it can be started while the person is still drinking.
While Naltrexone does not treat withdrawal symptoms, it plays a crucial role in helping individuals remain substance-free after the withdrawal period.
Side Effects and Considerations with Naltrexone
Naltrexone is generally well-tolerated, but it does come with potential side effects, including nausea, headaches, dizziness, and fatigue. More severe side effects can occur but are less common.
- It’s crucial to note that Naltrexone can cause severe or even life-threatening complications if opioids are used while on the medication.
- It’s also essential to inform healthcare providers of any liver issues, as Naltrexone can cause liver damage in certain circumstances.
- It should not be used by individuals who are pregnant, nursing, or planning to become pregnant.
Naloxone: The Emergency Responder
Unlike Naltrexone, Naloxone is not used as a long-term treatment for addiction. Instead, it is used in emergency situations to quickly reverse the effects of an opioid overdose.
Naloxone and its Role in Overdose Treatment
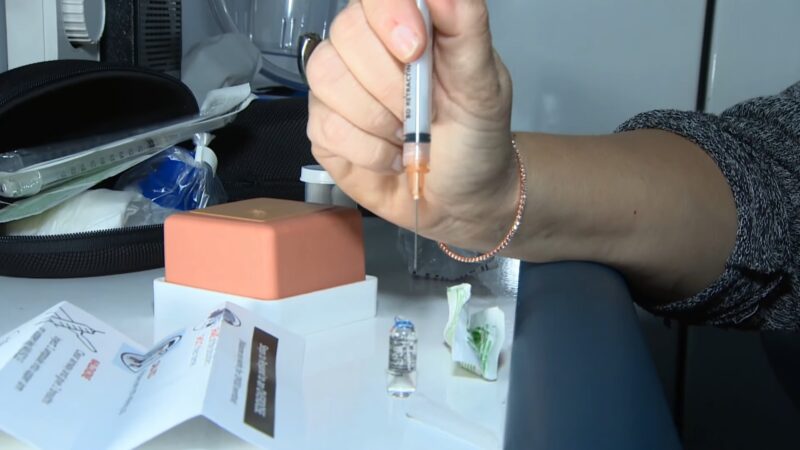
Naloxone acts rapidly, reversing the effects of an opioid overdose within minutes. It can be administered via injection or nasal spray, and its effects last between 30-90 minutes, buying time for medical professionals to provide further treatment.
- It’s important to note that Naloxone does not reverse overdoses from non-opioid drugs, such as benzodiazepines, cocaine, or alcohol.
- While Naloxone is a lifesaver in an overdose situation, it is not a substitute for professional medical treatment.
- It can cause withdrawal symptoms in individuals who have a physical dependence on opioids.
The ability of Naloxone to reverse an overdose rapidly has led to it being carried by first responders and made available over-the-counter in many places for use in emergencies.
Side Effects and Considerations with Naloxone

Like all medications, Naloxone can cause side effects. These may include body aches, fever, and rapid heart rate. It can also precipitate opioid withdrawal symptoms in those with a physical dependency on opioids, which, while not life-threatening, can be very uncomfortable.
- It’s vital to seek immediate medical attention after administering Naloxone, as its effects wear off faster than most opioids, and an overdose can recur.
- Although rare, some individuals may have an allergic reaction to Naloxone. Signs of an allergic reaction include hives, difficulty breathing, and swelling of the face, lips, tongue, or throat.
In exploring the distinctions between these two medications, you may also wonder about their effectiveness for pain management, which is precisely what our article on Naltrexone’s rapid pain relief delves into.
FAQs
What are Naltrexone and Naloxone?
Naltrexone and Naloxone are both medications used to treat opioid addictions. They belong to a class of drugs known as opioid antagonists.
What is the primary use of Naloxone?
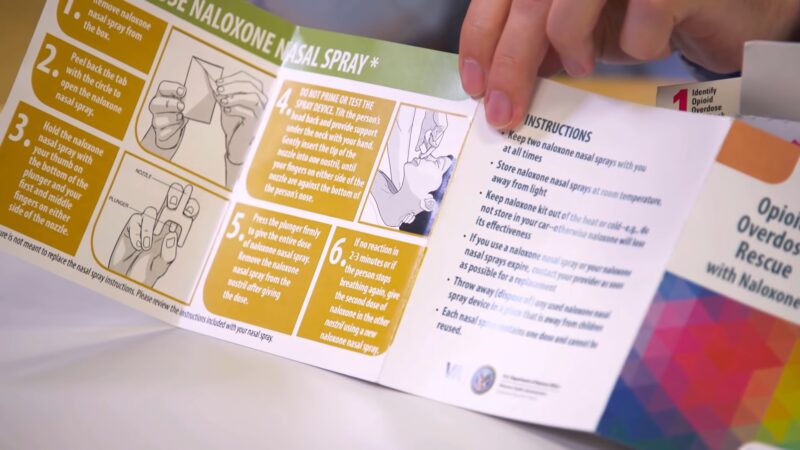
Naloxone is an emergency drug used to temporarily reverse the effects of an opioid overdose. It can be administered as a shot or nasal spray and can save lives if given quickly enough.
What is the primary use of Naltrexone?
Naltrexone is not an emergency drug. It is prescribed as part of a treatment plan to help individuals stop using drugs or consuming alcohol if they have a substance use disorder.
Can anyone administer Naloxone?
Yes, Naloxone can be given by anyone, not just healthcare professionals. It can be administered at home or on the street for a suspected overdose.
Can Naltrexone be used for alcohol addiction?
Yes, Naltrexone can be used as part of a treatment plan to block the “high” people seek when consuming alcohol. However, it doesn’t prevent the physical effects of alcohol consumption.
Can Naloxone be used if the type of drug taken is unknown?
Yes, Naloxone can be administered even if the type of drug taken is unknown. It will only work against opioids, but it won’t cause any harm if given to someone who doesn’t have opioids in their system.
Can Naltrexone be stopped abruptly?
No, Naltrexone should not be stopped without consulting with a doctor first, even if the individual is feeling better. Abruptly stopping the medication could lead to a relapse and the use of drugs or alcohol again.
Wrapping Up
While both Naltrexone and Naloxone are opioid antagonists used to counteract the effects of opioids, they serve different roles. Naltrexone is primarily a long-term treatment option for opioid and alcohol addiction, while Naloxone acts as an emergency antidote for opioid overdoses.
Both are crucial tools in our arsenal against the ongoing opioid epidemic, but understanding their differences is key to their effective use. As always, these medications should be used under the guidance of a healthcare provider, and any questions or concerns about them should be discussed with a medical professional.
